One-tube test could expand cervical cancer screening, speed diagnosis
University of Florida(UF) Health News
By Leah Buletti
Gainesville, Florida — Harnessing the power of CRISPR gene-editing technology in a new way, University of Florida researchers have created a one-tube testing method targeting DNA from body fluids that has the potential to dramatically increase access to the diagnosis of viral diseases such as cervical cancer.
Cervical cancer is among the most preventable cancers through vaccines or early detection tests. Early diagnosis significantly increases the chances that treatment of cancer will be successful or that irregular cells are found before they develop into cancer. Although effective vaccines that can prevent HPV infection are available, low vaccination rates persist, especially in Florida.
The simple platform uses a protein called Cas12a to analyze DNA in viruses such as HPV, which causes almost all cervical cancers. It can be paired with inexpensive devices using smartphones that test samples of body fluids such as blood or saliva, paving the way for new diagnostic tools that could have a major benefit in resource-limited areas or be used for at-home testing.
“Our assay is very promising to advance point-of-care testing for cervical cancer with minimal use of complex reagents and instruments,” said Yong Zeng, Ph.D., an associate professor in the department of chemistry and a member of the UF Health Cancer Center. “We developed a way to combine all processes into one material, making our method faster, simpler and more sensitive.”
Zeng led the study reporting the findings, published recently in the American Chemical Society’s journal ACS Applied Materials & Interfaces and funded by the National Cancer Institute, with He Yan, Ph.D., a postdoctoral scientist, and Zimu Tian, a graduate student.
Recently, CRISPR technology has been applied to various medical tests, but current tools mostly require a preamplification step to increase the target concentration before the virus can be detected. This step adds complexity and increases the risk of contamination during manual handling.
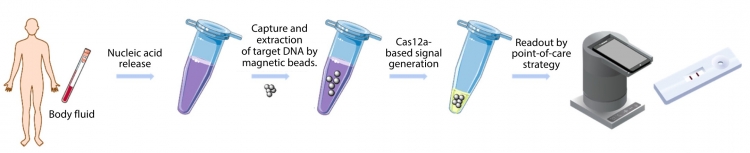
The UF researchers set out to design a preamplification-free CRISPR-Cas assay with high sensitivity and a simple workflow. In the test they came up with, target DNA is captured and extracted by magnetic beads coated with Cas12a/crRNA complexes called ribonucleoproteins.
Upon binding with the target, the ribonucleoproteins generate a signal that can be read by a lab instrument or paired with a portable device for a visualized readout. One of the portable devices the team tested is a low-cost platform that uses a smartphone to read the fluorescence signal.
The team tested how the assay, called SPEEDi-CRISPR, performed in detecting two high-risk HPV subtypes: HPV-16 and HPV-18, which account for about 70% of all cervical cancers. They found it could detect the two subtypes with high sensitivity and excellent specificity.
“We found it quite exciting that we could improve the sensitivity so much that we did not need the preamplification steps,” Zeng said.
The researchers believe the assay could also be used for other diseases and cancers caused by viruses, such as hepatitis C, a viral infection of the liver.
The discovery is the latest advancement in next-generation diagnostics based on gene-editing tools made by Zeng’s lab. Last year, the team developed a “one-pot” CRISPR assay called “EXTRA-CRISPR” for detecting microRNAs that could help clinicians diagnose cancer at earlier stages through blood tests.
The team plans to continue adapting its assays for other biologically significant targets, such as mRNA. They hope to collaborate with engineers to develop a fully automated small device to make the point-of-care tool more user-friendly for possible commercial applications.
Top
By Leah Buletti
Gainesville, Florida — Harnessing the power of CRISPR gene-editing technology in a new way, University of Florida researchers have created a one-tube testing method targeting DNA from body fluids that has the potential to dramatically increase access to the diagnosis of viral diseases such as cervical cancer.
Cervical cancer is among the most preventable cancers through vaccines or early detection tests. Early diagnosis significantly increases the chances that treatment of cancer will be successful or that irregular cells are found before they develop into cancer. Although effective vaccines that can prevent HPV infection are available, low vaccination rates persist, especially in Florida.
The simple platform uses a protein called Cas12a to analyze DNA in viruses such as HPV, which causes almost all cervical cancers. It can be paired with inexpensive devices using smartphones that test samples of body fluids such as blood or saliva, paving the way for new diagnostic tools that could have a major benefit in resource-limited areas or be used for at-home testing.
“Our assay is very promising to advance point-of-care testing for cervical cancer with minimal use of complex reagents and instruments,” said Yong Zeng, Ph.D., an associate professor in the department of chemistry and a member of the UF Health Cancer Center. “We developed a way to combine all processes into one material, making our method faster, simpler and more sensitive.”
Zeng led the study reporting the findings, published recently in the American Chemical Society’s journal ACS Applied Materials & Interfaces and funded by the National Cancer Institute, with He Yan, Ph.D., a postdoctoral scientist, and Zimu Tian, a graduate student.
Recently, CRISPR technology has been applied to various medical tests, but current tools mostly require a preamplification step to increase the target concentration before the virus can be detected. This step adds complexity and increases the risk of contamination during manual handling.
The UF researchers set out to design a preamplification-free CRISPR-Cas assay with high sensitivity and a simple workflow. In the test they came up with, target DNA is captured and extracted by magnetic beads coated with Cas12a/crRNA complexes called ribonucleoproteins.
Upon binding with the target, the ribonucleoproteins generate a signal that can be read by a lab instrument or paired with a portable device for a visualized readout. One of the portable devices the team tested is a low-cost platform that uses a smartphone to read the fluorescence signal.
The team tested how the assay, called SPEEDi-CRISPR, performed in detecting two high-risk HPV subtypes: HPV-16 and HPV-18, which account for about 70% of all cervical cancers. They found it could detect the two subtypes with high sensitivity and excellent specificity.
“We found it quite exciting that we could improve the sensitivity so much that we did not need the preamplification steps,” Zeng said.
The researchers believe the assay could also be used for other diseases and cancers caused by viruses, such as hepatitis C, a viral infection of the liver.
The discovery is the latest advancement in next-generation diagnostics based on gene-editing tools made by Zeng’s lab. Last year, the team developed a “one-pot” CRISPR assay called “EXTRA-CRISPR” for detecting microRNAs that could help clinicians diagnose cancer at earlier stages through blood tests.
The team plans to continue adapting its assays for other biologically significant targets, such as mRNA. They hope to collaborate with engineers to develop a fully automated small device to make the point-of-care tool more user-friendly for possible commercial applications.