Patients who recover from severe COVID-19 still have significant risk of death, UF study finds
UF Health Communications
By Jill Pease
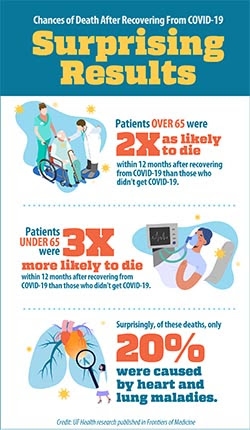
Gainesville, Florida - Patients who have recovered from severe COVID-19 have more than twice the mortality risk within the year following their illness than people who have not contracted the virus.
The study by University of Florida researchers, who previously reported that patients who had a severe case of the disease were more than twice as likely to need rehospitalization for COVID-19 complications, underscores the serious effects the virus can have on the body. The study appears in the journal Frontiers in Medicine.
“These findings reinforce that the internal trauma of being sick enough to be hospitalized with COVID-19 has a big consequence for people’s health. This is a huge complication of COVID-19 that has not been shown before,” said Arch G. Mainous III, Ph.D., the study’s lead investigator and a professor in the department of health services research, management and policy at the UF College of Public Health and Health Professions, part of UF Health.
“Our findings suggest the need for closer follow-up of patients who have been hospitalized with COVID in the same way we keep a close eye on people who are at risk for heart attack,” Mainous added. “COVID-19 is even more devastating than we thought when only focusing on the initial episode. The downstream risk for the most severe outcome, death, is definitely high enough to hopefully make everyone rethink the impact of COVID-19.”
The UF team analyzed data from electronic health records of 13,638 adult patients at one health system who were tested for COVID-19 using a polymerase chain reaction, or PCR, test. The researchers then followed patients for 12 months.
Among the group, 178 had severe COVID-19 requiring hospitalization and 246 patients had mild or moderate COVID-19. The rest tested negative for COVID-19. The researchers excluded data on deaths 30 days after patients’ recovery from COVID-19 to ensure that any deaths recorded during that window were not caused by the initial illness. After adjusting for factors including age, race, gender and select existing medical conditions, patients who had recovered from severe COVID-19 were 233% more likely to die within a year after infection than patients who had tested negative for COVID-19.
The researchers were surprised to find that among patients who had severe COVID-19 and later died, deaths attributed to cardiovascular, respiratory and clotting problems - common complications of COVID-19 infection - only accounted for 20% of deaths. The discovery that these patients died from a variety of conditions is a critical area for further study, the authors say.
The researchers also found that patients younger than 65 who recovered from severe COVID-19 were at greater risk of dying than patients over 65 who had been hospitalized with severe COVID-19, when compared with COVID-19-negative counterparts.
The researchers stress that vaccination is the most effective way to decrease the risk of hospitalization and death from COVID-19.
“A lot of battles are raging over whether to get vaccinated for COVID-19,” said Mainous, also vice chair for research in the UF College of Medicine’s department of community health and family medicine. “Patients may feel that if they are hospitalized and recover from COVID-19 then they have beaten COVID-19. Unfortunately, having a substantially increased of death in the next year after recovery from a severe episode of COVID-19 shows that this is not the case. Preventing severe COVID-19 should be our primary focus.”
In addition to Mainous, the research team included Benjamin J. Rooks, M.S., a clinical research coordinator; Velyn Wu, M.D., an assistant professor; and Frank A. Orlando, M.D., an assistant professor and assistant medical director, all from the department of community health and family medicine at the UF College of Medicine. The research was supported by funding from the National Center for Advancing Translational Sciences of the National Institutes of Health under University of Florida Clinical and Translational Science awards.
Top
By Jill Pease
Gainesville, Florida - Patients who have recovered from severe COVID-19 have more than twice the mortality risk within the year following their illness than people who have not contracted the virus.
The study by University of Florida researchers, who previously reported that patients who had a severe case of the disease were more than twice as likely to need rehospitalization for COVID-19 complications, underscores the serious effects the virus can have on the body. The study appears in the journal Frontiers in Medicine.
“These findings reinforce that the internal trauma of being sick enough to be hospitalized with COVID-19 has a big consequence for people’s health. This is a huge complication of COVID-19 that has not been shown before,” said Arch G. Mainous III, Ph.D., the study’s lead investigator and a professor in the department of health services research, management and policy at the UF College of Public Health and Health Professions, part of UF Health.
“Our findings suggest the need for closer follow-up of patients who have been hospitalized with COVID in the same way we keep a close eye on people who are at risk for heart attack,” Mainous added. “COVID-19 is even more devastating than we thought when only focusing on the initial episode. The downstream risk for the most severe outcome, death, is definitely high enough to hopefully make everyone rethink the impact of COVID-19.”
The UF team analyzed data from electronic health records of 13,638 adult patients at one health system who were tested for COVID-19 using a polymerase chain reaction, or PCR, test. The researchers then followed patients for 12 months.
Among the group, 178 had severe COVID-19 requiring hospitalization and 246 patients had mild or moderate COVID-19. The rest tested negative for COVID-19. The researchers excluded data on deaths 30 days after patients’ recovery from COVID-19 to ensure that any deaths recorded during that window were not caused by the initial illness. After adjusting for factors including age, race, gender and select existing medical conditions, patients who had recovered from severe COVID-19 were 233% more likely to die within a year after infection than patients who had tested negative for COVID-19.
The researchers were surprised to find that among patients who had severe COVID-19 and later died, deaths attributed to cardiovascular, respiratory and clotting problems - common complications of COVID-19 infection - only accounted for 20% of deaths. The discovery that these patients died from a variety of conditions is a critical area for further study, the authors say.
The researchers also found that patients younger than 65 who recovered from severe COVID-19 were at greater risk of dying than patients over 65 who had been hospitalized with severe COVID-19, when compared with COVID-19-negative counterparts.
The researchers stress that vaccination is the most effective way to decrease the risk of hospitalization and death from COVID-19.
“A lot of battles are raging over whether to get vaccinated for COVID-19,” said Mainous, also vice chair for research in the UF College of Medicine’s department of community health and family medicine. “Patients may feel that if they are hospitalized and recover from COVID-19 then they have beaten COVID-19. Unfortunately, having a substantially increased of death in the next year after recovery from a severe episode of COVID-19 shows that this is not the case. Preventing severe COVID-19 should be our primary focus.”
In addition to Mainous, the research team included Benjamin J. Rooks, M.S., a clinical research coordinator; Velyn Wu, M.D., an assistant professor; and Frank A. Orlando, M.D., an assistant professor and assistant medical director, all from the department of community health and family medicine at the UF College of Medicine. The research was supported by funding from the National Center for Advancing Translational Sciences of the National Institutes of Health under University of Florida Clinical and Translational Science awards.